35 yr old male with fever,since 2 months and bicytopenia
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
35 yr old male who works for oil factory as supervisor
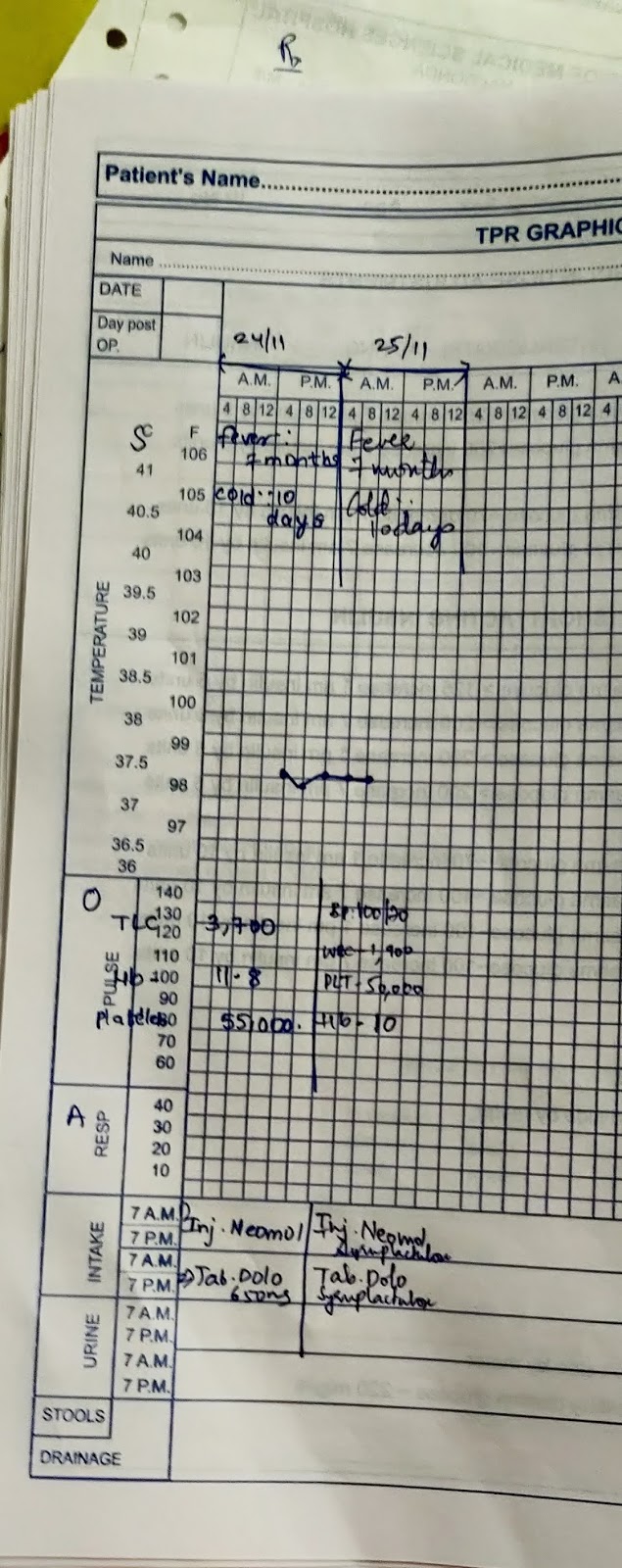
Patient had chief complaints of fever since 2 months on and off , low grade fever,increased during night,relieved on medication; gradual onset; associated with chills, pt had been feeling cold since 10 days.
No complaints of cough, abdominal pain, dysphagia, head ache,burning micturition,
Patient had complaints of weight loss approximately 7 kgs since 2 months
Patient had no H/O vomitings, nausea.
Complaints of decreased appetite associated with indigestion
Patient had complaints of constipation , passing stools once for 6-7 days
No wounds,abscess or skin infections
History of present illness: no c/o SOB, orthopnea, syncope.
No c/o chest pain, palpitations
C/o headache during episode of fever on right temporal side
No c/o burning micturition.
History of past illness: not a k/c/o DM, HTN, epilepsy, asthma,TB.
Personal history:
Appetite: decreased
Bowels: irregular , passing stools once for 5-7 days
Bladder movements - normal
alcholic since 10 years 90ml / 2 days last binge was 7 months back.. and abstinence since 2 months
Non smoker but takes chewable tobacco 1 packet for 5 days
Family history:
No history of DM, HTN CAD, CVA, aasthma in the family
General examination: patient is conscious, coherent, cooperative
Pallor is seen.
No icterus, cyanosis, clubbing,lymphadenopathy, edema
Vitals:
Temp:98.5F
Pulse: 80bpm
Respiratory rate: 19/ min
Bp: 110/80 mm hg
SpO2-99% in room air
Systemic examination:
vs: S1 S2 heard no additional sounds or murmurs
Rs: NVBS
Abdomen: soft,non tender
Cns: higher mental functions intact
Provisional diagnosis: fever with bicytopenia















Comments
Post a Comment